HIPAA and HL7 Messaging
HL7 messages are typically exchanged between enterprise applications such as a Patient Administration System and a Pathology Laboratory Information system. However, HL7 messages must sometimes be embedded in certain HIPAA EDI-X12 transactions between enterprises such as hospitals and insurance companies.
For example, when a hospital sends a claim for payment to another enterprise, such as an insurance company, the hospital and the insurance company exchange HIPAA EDI-X12 messages. HIPAA EDI-X12 messages might contain an embedded HL7 message with additional patient information requested from the insurance company.
TIBCO HL7/HIPAA Solution
To enable the exchange of HIPAA messages with HL7 attachments between enterprises, TIBCO offers:
- ActiveMatrix BusinessWorks Plug-in for HL7 with FHIR, the TIBCO implementation of the HL7 standard. It provides a framework for a healthcare provider's internal HL7 HIPAA messaging.
- TIBCO BusinessConnect™ EDI Protocol HIPAA Edition powered by Instream®, the TIBCO implementation of the EDI standard. It offers specialized functionality for customers who require HIPAA compliance.
Together, these products enable the exchange of HIPAA messages and embedded HL7 messages between enterprises such as hospitals and insurance companies.
Sample High-Level Scenario
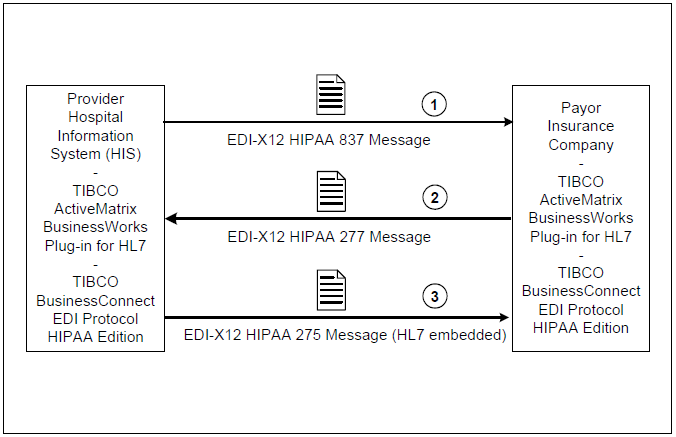
These two products can be used in concert to provide the ability to include HL7 information in EDI-X12 275 HIPAA messages exchanged between a healthcare enterprise and an external payer enterprise.
The following figure shows how the message exchange occurs:
- You use BusinessConnect EDI Protocol HIPAA Edition powered by Instream to send an EDI-X12 837 Health Care Claim HIPAA message to an external payer.
- The payer uses BusinessConnect EDI Protocol HIPAA Edition powered by Instream to send an EDI-X12 277 Health Care Information Status Notification HIPAA message back to you. This is a responder request for more information.
- You use BusinessConnect EDI Protocol HIPAA Edition powered by Instream to send an EDI-X12 275 Patient Information HIPAA message back to the payer. This is a responder response message.
The BIN segment of this 275 XML message contains an embedded HL7 ORU (Observation Result/Unsolicited) message created in ActiveMatrix BusinessWorks Plug-in for HL7 with FHIR with the additional patient information that was requested. This information can include diagnoses, test results, observations, and treatments.
The BIN segment is carried in the response field of the private RESPONDER.RESPONSE message in EDI HIPAA. See the TIBCO BusinessConnect™ EDI Protocol HIPAA Edition Guide for more information on the RESPONDER.RESPONSE messaging class. The embedded HL7 ORU message is obtained during EDI processing in TIBCO ActiveMatrix BusinessWorks. Also see HL7 ORU Messages.
There are many other scenarios where it makes sense to use ActiveMatrix BusinessWorks Plug-in for HL7 with FHIR and BusinessConnect EDI Protocol HIPAA Edition powered by Instream together. For example, after a patient is discharged, the HL7 discharge message can trigger queries to a billing system, which can then generate a proper 837 HIPAA message to send to the insurance company. This streamlines the operation for claim submission, brings valuable turn-around time for the provider, and helps increase efficiency and return on investment.
Provider and Payer Roles When Sending an EDI-X12 275 HIPAA Message
- Express patient data as an HL7 ORU message.
- Use the appropriate LOINC (Logical Observation Identifier Names and Codes) modifier code.
- Wrap the HL7 ORU message in the BIN segment of an X12N-compliant 275 claims attachment transaction. X12N is for exchanging insurance, eligibility, and managed care information.